Blood Cancer : 5 Types of Blood Cancer, Stages and Adequate Information
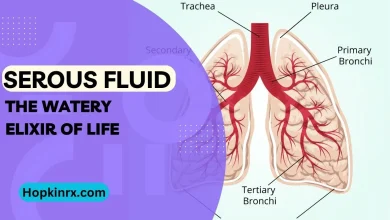
Types of blood cancer
Information about blood cancers and blood disorders, including diagnosis and treatment.

1. Leukaemia
What is leukaemia?
Leukemia is the overall name given to a gathering of tumors created in the bone marrow. Leukemia starts in creating platelets that have gone through a dangerous change. This implies that they duplicate in an uncontrolled manner and don’t develop as expected, leaving them incapable to work as they ought to.
Most instances of leukemia begin in creating white cells. In a few cases, leukemia creates in other blood-framing cells, for instance in creating red cells or creating platelets. Leukemia can likewise be either myeloid or lymphocytic. The terms myeloid and lymphocytic allude to the sorts of cells wherein leukemia initially began. Myeloid foundational microorganisms form into red cells, white cells (neutrophils, eosinophils, basophils, and monocytes), and platelets. Lymphoid foundational microorganisms create in two different sorts of white cells called T-lymphocytes and B-lymphocytes.
The two grown-ups and kids can foster leukemia however particular sorts are more normal in various age gatherings.
Type of leukemia
There are a few distinct sorts and subtypes of leukemia. Leukemia can be either intense or ongoing.
Under typical conditions, the bone marrow contains few juvenile cells, called impact cells. These youthful impact cells form into mature white cells, red cells, and platelets which are ultimately delivered into the circulation system.
In individuals with intense leukemia , the sick bone marrow delivers an unreasonable number of unusual impact cells, called leukaemic cells. These phones collect in the bone marrow meddling with the creation of typical platelets. Intense leukemia creates and advances rapidly and in this way should be treated when it is analyzed.
Common forms of acute leukaemia are:
Acute myeloid leukaemia (AML)
Information about AML
Acute lymphoblastic leukaemia (ALL)
Information about ALL
Acute promyelocytic leukaemia (APML)
Information about APML
In constant leukemia there is an amassing of mature yet strange white platelets that have gone through a threatening change when creating from an impact cell. Ongoing leukemia advances more leisurely than intense leukemia and may not need therapy for quite a while after it is analyzed.
Common forms of chronic leukaemia are:
Chronic myeloid leukaemia (CML)
Chronic myeloid leukaemia (CML)
Chronic lymphocytic leukaemia (CLL)
Chronic lymphocytic leukaemia (CLL)
Hairy cell leukaemia (HCL)
Hairy cell leukaemia
Other types of uncommon leukaemia
Biphenotypic leukaemia
Biphenotypic leukaemia
2. Lymphoma
What is lymphoma?
Lymphoma is the overall term for malignant growths create in the lymphatic framework. The lymphatic framework is comprised of an immense organization of vessels (like veins) that branch out into every one of the tissues of the body. These vessels contain lymph, a dismal watery liquid that conveys lymphocytes, which are specific white platelets that battle the disease. There are two kinds of lymphocytes, B-lymphocytes and T-lymphocytes (additionally called B-cells and T-cells). These cells ensure us by making antibodies and annihilating unsafe microorganisms like microbes and infections.
Lymphoma starts in creating B-lymphocytes and T-lymphocytes, which have gone through a dangerous change. This implies that they increase with no legitimate request, shaping growths which are assortments of disease cells. These cancers cause an expansion in the lymph hubs and different pieces of the body.
After some time, dangerous lymphocytes (called lymphoma cells) swarm out typical lymphocytes and at last, the insusceptible framework becomes debilitated and can presently don’t work as expected. Huge advances are persistently being made in the manner your lymphoma can be overseen. This implies that with treatment, many individuals would now be able to be relieved. Numerous other people who are dealt with remain infection-free and well for quite a while.
Sub-types of lymphoma
There are in excess of 80 diverse sub-sorts of lymphoma right now perceived by the World Health Organizations’ order framework.
Five of these sub-types have a place with a gathering of illnesses called Hodgkin lymphoma. Any remaining sub-types are normally gathered and called non-Hodgkin lymphomas.
Sub-types of lymphoma
Non-Hodgkin lymphoma
Hodgkin lymphoma
Types of blood cancer
3. Myeloma
What is myeloma?

Myeloma is a malignant growth of the plasma cells. Plasma cells are experienced lymphocytes (a kind of white platelet) that assist with battling the disease by delivering extraordinary proteins known as antibodies or immunoglobulins. Immunoglobulins (Ig) are delivered by plasma cells in light of microbes, infections, and other unsafe substances found in the body.
Myeloma creates when plasma cells go through a harmful or threatening change and become myeloma cells. These myeloma cells increase with practically no legitimate request and structure assortments known as growths that aggregate in various pieces of the body, particularly in the bone marrow and on the surfaces of various bones in the body. These growths emit synthetics that invigorate other bone marrow cells (osteoclasts) to eliminate calcium from the bone. Thus bones can become more vulnerable, weaker and break all the more without any problem.
As myeloma cells duplicate, they swarm the bone marrow and keep it from making ordinary quantities of red cells (causing iron deficiency), white cells (expanding your weakness to contaminations), and platelets (expanding your defenselessness to draining and swelling). Myeloma cells can likewise meddle with the development of typical antibodies. Myeloma cells produce an unusual kind of immunoglobulin called paraprotein (otherwise called monoclonal immunoglobulin, myeloma protein, or basically M protein). At times an unnecessary number of sections of immunoglobulin known as light chains are delivered. These light chains can be identified in the blood and they likewise show up in the pee. Light chains identified in the pee are called Bence-Jones protein.
What are the stages and kinds of myeloma?
Knowing the specific phase of your sickness is significant in light of the fact that it gives more data about the probable course of your infection (guess) and the most ideal method for treating it. Myeloma can be ordered by how the infection is circulated in your body. The International Staging System (ISS) depends on two tests and characterizes three phases of myeloma:
Stage I is early sickness
Stage II is in the middle of Stage I and Stage III
Stage III is progressed sickness, where there is a lot of myeloma in the body.
The CRAB rules are regularly used to distinguish whether an individual has dynamic myeloma, which might require treatment. The abbreviation CRAB comprises of (C) expanded calcium level (R) renal (kidney) issues (A) paleness and (B) bone changes (lytic sores or bone misfortune). At least one of these CRAB side effects demonstrates indicative myeloma, which requires treatment. In most cases, myeloma is found in different bone marrow locales at analysis, which is the reason the sickness is regularly called numerous myeloma. Now and then a disconnected assortment of myeloma cells is found in just one site. At the point when this happens,, the sickness is portrayed as singular myeloma or single plasmacytoma. Plasmacytomas can in some cases be effectively treated utilizing radiotherapy alone read more with regards to them here.
Certain individuals have an expanded number of plasma cells in their bone marrow, however don’t fit the rules for analysis of numerous myeloma. Their sickness might be named MGUS or seething myeloma:
Monoclonal gammopathy of unsure importance (MGUS) is a non-harmful (non-malignant) condition identified with myeloma. It additionally includes the development of paraprotein by plasma cells. MGUS doesn’t cause any indications and it is normally gotten during a standard blood or pee test Individuals determined to have MGUS don’t need any treatment separated from ordinary development by their PCP, normally consistently to have their protein levels checked. Over the long run,, few individuals with MGUS will foster myeloma. Peruse more with regards to MGUS here.
More information about Types of blood cancer
Seething myeloma is a beginning stage of myeloma without any manifestations, however,, a bone marrow biopsy shows unequivocal proof of myeloma. Individuals determined to have seething myeloma needn’t bother with treatment straight away. Treatment is given at a later stage when the illness advances after certain months or a long time.
How common is myeloma?
Myeloma is a generally uncommon sickness. It represents roughly 1% of all tumors and 10% of all blood and bone marrow diseases. Every year in Australia around 1,500 individuals are determined to have myeloma.
Who gets myeloma?
Myeloma basically influences more seasoned individuals, with a normal age of 70 years at the hour of analysis. Seldom, myeloma can influence individuals in their 20s and 30s. Myeloma is more normal in men than in ladies.
What causes myeloma?
The reason for myeloma remains primarily obscure. You can’t get myeloma by being in touch with somebody who has it. There are uncommon situations where myeloma happens in families, however in by far most cases individuals who are determined to have myeloma have no family background of the infection. There are sure factors that might put certain individuals at a higher danger of treating myeloma. These incorporate openness to high portions of radiation and continuous openness to specific modern or natural synthetic compounds. Certain individuals with MGUS will ultimately proceed to foster myeloma.
What are the symptoms of myeloma?
The manifestations of myeloma rely upon how best in class the illness is. In the soonest organizes, there might be no manifestations,, and myeloma is gotten during a normal blood test. The most widely recognized indication of myeloma is bone agony. This is generally felt toward the back or ribs and might be aggravated by development. Bone agony is generally the consequence of the steady disintegration of bone brought about by substances emitted by myeloma cells. Over the long run bones can become debilitated and diminished (osteoporosis) and openings (lytic injuries) may create, expanding the danger of crack (the bone-breaking). At the point when bone tissue is harmed, calcium is let out of the bone into the circulation system. An abundance of calcium in the blood is called hypercalcemia. If you have a higher than ordinary calcium level in your blood you might feel disgusted, blocked up, drained, parched, or even befuddled.
There are many reasons for kidney harm in myeloma. The paraprotein created by the myeloma cells can harm the kidneys. This is particularly the situation when the Bence Jones protein is involved. Different factors, for example, parchedness and hypercalcemia can likewise cause kidney harm. The indications of this might incorporate weariness, mental disarray, enlarged lower legs, and changed urinary yield. Different manifestations of myeloma emerge when these malignant growth cells swarm the bone marrow and keep it from making ordinary platelets and may include:
frailty because of an absence of red cells and causing constant sleepiness, wooziness, pallor, or windedness when truly dynamic
incessant or rehashed contaminations and slow mending because of an absence of typical white platelets, particularly neutrophils
expanded or unexplained draining or swelling because of an extremely low platelet count.
More information about myeloma
- Myeloma diagnosis
- Myeloma treatment and side effects
- Solitary plasmacytoma
- Monoclonal gammopathy of unknown significance (MGUS)
- Bisphosphonates
- Other Myeloma Resources
4. Myelodysplastic syndromes (MDS)
What is MDS?
Myelodysplastic conditions (MDS, or myelodysplasia) are a gathering of blood diseases that all affect, to a more prominent or lesser degree, the creation of typical platelets in the bone marrow. These incorporate ongoing myelomonocytic leukemia (CMML), adolescent myelomonocytic leukemia (JMML), abnormal persistent myeloid leukemia (CML), and myelodysplastic/myeloproliferative neoplasms unclassifiable (MDS/MPN). MDS happens because of a transformation (or change) in at least one of the qualities that control platelet improvement. This change or change brings about the strange development of blood undeveloped cells.
The first change is safeguarded when the impacted undifferentiated organism partitions and delivers a clone; that is, a gathering of indistinguishable cells all with a similar imperfection. This is the reason MDS is here and there depicted as a clonal blood undifferentiated organism issue. Transformations in isolating cells happen constantly and cells have sharp methods of shutting down these anomalies continuing and creating issues inside the body. The more we live, notwithstanding, the more possibility we have of securing changes that figure out how to get away from these protected watchmen. That is the reason MDS, as most leukemias and different diseases, turns out to be more normal as we get more established. This normally happening or immediately emerging MDS is alluded to as essential MDS.
In MDS, unusual bone marrow undifferentiated organisms (called impact cells) produce expanded quantities of youthful platelets. These cells don’t develop as expected and frequently bite the dust rashly. This outcome in lower quantities of mature red platelets, white platelets, and platelets being created. The platelets that do endure are frequently of low quality, are unusual in shape (dysplastic), and can’t work as expected. This implies that individuals with MDS frequently have an extremely dynamic bone marrow yet a low number of flowing platelets. Without enough red platelets, white platelets, and platelets you can become exhausted, more defenseless to contaminations, and too draining and swelling all the more without any problem.
Which kind of MDS do I have?
There are various kinds of MDS that can shift in seriousness and how much typical platelet creation is impacted. Individuals with gentle infection are regularly found to just be pale, or they may have a lower than ordinary white platelet or platelet count, yet by and large, they have hardly any, alarming manifestations from their sickness. In more extreme cases, the absence of circling platelets is more articulated, causing more indications.
The current World Health Organization’s characterization framework perceives a few significant subtypes of MDS. These subtypes are recognized from one another by how much ordinary platelet creation is impacted, the number of impact cells present, and the probability of change into intense myeloid leukemia. Knowing the specific kind of MDS you have is significant on the grounds that it assists the specialist with settling on the best course of treatment to suggest for you.
Types of blood cancer
Refractory anaemia (RA)
In this kind of MDS, the red platelets are generally impacted, causing frailty. The bone marrow contains under 5% strange impact cells and there are none found in the circling blood. This kind of MDS once in a while changes to leukemia and treatment is customary perception of blood bonding as it were.
Myelodysplastic syndrome with del (5q) chromosome
Red platelets are impacted, causing pallor. There are normally under 5% shoot cells in the bone marrow and coursing blood and it is related with a decent visualization.
Refractory anaemia with ringed sideroblasts (RARS)
Like RA, however, for this situation, the red platelets can’t deal with the iron that ordinarily goes into making hemoglobin, the oxygen-conveying part of the red cell. Rather the iron granules are stored such that frames a ring around the core of a creating red platelet this is known as a ringed sideroblast.
Refractory anaemia with excess blasts – type 1 (RAEB-1)
At least one platelet type is impacted. The bone marrow contains somewhere in the range of 5% and 9% impact cells and there are just a few impact cells (under 5%) found in the flowing blood.
Refractory anaemia with excess blasts – type 2 (RAEB-2)
At least one platelet type is impacted, however, this time the bone marrow contains somewhere in the range of 10% and 19% impact cells, and the number likewise increments (somewhere in the range of 5% and 19%) in the circling blood. There is a more noteworthy probability of changing to intense myeloid leukemia.
Refractory cytopenia with multilineage dysplasia (RCMD)
At least two platelet types are typically impacted here however again the bone marrow contains under 5% impact cells, and there are generally none found in the coursing blood.
Refractory cytopenia with multilineage dysphasia and ringed sideroblasts (RCMDRS)
Like RCMD, yet with ringed sideroblasts found in the red platelets.
Myelodysplastic/myeloproliferative neoplasms (MDS/MPN)
These are a gathering of sicknesses that have attributes of both myelodysplastic (unusual bone marrow cells creating too barely any platelets) and myeloproliferative (strange bone marrow cells delivering too many platelets) neoplasms. These incorporate ongoing myelomonocytic leukemia (CMML), adolescent myelomonocytic leukemia (JMML), abnormal constant myeloid leukemia (aCML) and myelodysplastic/myeloproliferative neoplasms unclassifiable (MDS/MPN).
How normal is MDS?
By and large, MDS is generally phenomenal, with a frequency of between four to five for each 100,000 of the populace. Notwithstanding, in patients beyond 60 20 years old, increments to anything from 20 to 50 for each 100,000. It is accordingly one of the more normal hematological problems in the old.
It is hard to make certain of the specific number of individuals who have MDS. This is on the grounds that much of the time the illness grows gradually and individuals don’t have any indications for quite a while.
Who gets MDS?
While MDS can happen at whatever stage in life, most cases (more than 90%) create beyond 60 years old. MDS can happen incidentally in kids.
Types of blood cancer
What causes MDS?
Why imperfections emerge in the bone marrow and cause MDS in a specific individual at a specific time is hard to comprehend, albeit the impacts of maturing on cell development seem to assume a significant part. Any cycle which harms qualities and prompts changes might play a part in the advancement of MDS. There are additionally some perceived variables that might put certain individuals at a higher danger of creating MDS:
- maturing has all the earmarks of being the main danger factor for MDS on the grounds that the danger of creating transformations increments with age
- openness to significant levels of some ecological synthetic substances, particularly benzene and oil based goods
- openness to synthetic compounds in tobacco smoke
- individuals recently treated for disease or different conditions with chemotherapy are at an expanded danger of creating what is called optional or treatment-related MDS. This records for under 10% of all instances of MDS
- past radiation treatment, or inadvertent openness to significant degrees of natural illumination
- individuals with specific innate issues, for example, Blooms Syndrome, Downs Syndrome, Fanconi pallor and neurofibromatosis can have shaky qualities and are more in danger of creating changes that cause MDS or disease.
What are the manifestations of MDS?
Many individuals in the beginning phases of MDS have no indications by any means and it is gotten unintentionally during a standard blood test. In different cases, individuals go to see their General Practitioner since they are encountering some upsetting manifestations. The sorts of indications that individuals experience rely upon how serious their illness is and the kind of platelet that is generally impacted.
The most well-known manifestations are brought about by an absence of red cells, or pallor:
- determined sleepiness and weariness
- shortcoming
- windedness with insignificant exercise
- looking pale.
Types of blood cancer
Unusual white cell work, regularly with low white cell counts, causes:
- repeating diseases, particularly chest contaminations
- fevers
- sore mouth because of mouth ulcers.
Strange platelet work, regularly with low platelet counts, causes:
- simple swelling
- purpura a rash of little red dabs, seen regularly on the lower appendages at first, because of little shallow hairlike drains which are known as petechiae
- propensity to drain from the nose and gums.
Many individuals with MDS have a blend of side effects. This is on the grounds that the creation of all of the platelet types might be impacted by the sickness. A portion of these indications may likewise be seen in different ailments, including viral contaminations. See your primary care physician if you have any indications that don’t disappear so you can be inspected and treated appropriately.
More about various types of MDS
- Chronic myelomonocytic leukaemia
- Deletion 5q
- RAEB
- MDS – RARS
- MDS – RCMD
- MDS – RCUD
More information about MDS
- MDS diagnosis
- MDS treatment and side effects
5. Myeloproliferative neoplasms (MPN)
What is MPN?
Myeloproliferative neoplasms (MPN) are malignant growths that begin in the bone marrow, where platelets are made.
In MPN, the bone marrow makes an excessive number of at least one sort of platelet (red platelets, white platelets as well as platelets). These cells change the thickness of the blood. Now and again they don’t work appropriately. They likewise swarm the bone marrow and afterward,, it cannot make sufficient solid platelets.
There are seven sorts of MPN, analyzed utilizing blood tests and a bone marrow biopsy. A few structures can change into different sorts of MPN or into intense myeloid leukemia.
Indications rely upon which kind of MPN you have. Manifestations normal to the kinds are exhaustion, shortcoming, weight reduction, developed spleen (splenomegaly), swelling and dying, night sweats, torment in bones or joints.
By and large, we don’t realize what causes MPN. There is typically a transformation in (change to) the hereditary material of developing platelets. There is no real way to forestall MPN and you cannot get it or pass it on.
How normal is MPN?
Myeloproliferative neoplasms are an uncommon gathering of blood diseases. Polycythaemia vera is analyzed in an expected 250 Australians every year, fundamental thrombocythaemia around 200,, and myelofibrosis an expected 150. The more extraordinary sub sorts of MPN, collectively, are analyzed in under 50 Australians each year.
Who gets MPN?
The vast majority with an MPN have no family ancestry. MPN is all the more regularly analyzed in individuals beyond 50 years old in spite of the fact that it can once in a while happen in more youthful individuals, even infrequently in youngsters.
What causes MPN?
The specific reason for MPNs stay obscure yet there are probably going to be various elements included. That is the reason MPNs, as most leukemias and different tumors become more normal as we get more established. A transformation of a specific quality (a fragment of DNA that makes proteins) known as Janus kinase 2 (JAK2) is found in a huge extent of individuals with MPNs. The specific significance of this change stays muddled yet it seems to assume a part in the overproduction of platelets found in these problems. The revelation of a change in the JAK2 quality is significant in light of the fact that it is probably going to fundamentally affect the manner in which MPNs are analyzed and treated.
Long haul openness to undeniable degrees of benzene or extremely high portions of ionizing radiation might expand the danger of myelofibrosis in a few cases. Around 33% of individuals with myelofibrosis have been recently determined to have polycythemia or fundamental thrombocythaemia.
What are the indications of MPN?
Many individuals have no side effects when they are first determined to have an MPN and the sickness is gotten incidentally during a normal blood test or actual assessment. In different cases, individuals go to see their GP since they make them inconvenience side effects of their infection. At the point when side effects do happen, they foster progressively after some time. Normal indications include:
- headaches
- blurred vision
- fatigue
- weakness
- dizziness
- itchiness (pruritus)
- night sweats
- raised blood pressure (hypertension).
Types of MPN
Polycythaemia (rubra) vera
Amplification of the spleen (splenomegaly) is normal and happens in around 75% of cases. Now and again the liver may likewise be expanded: this is called hepatomegaly. Certain individuals experience gout, which typically presents as an excruciating aggravation of the large toe or foot. A few people might create erythromelalgia, an uncommon condition described by serious consuming torment of impacted furthest points and an expanded skin temperature. By and large, individuals with PV have a bronzed (red) coloring and blushing of the centers of their hands, the bottoms of their feet, ear flaps, mucous layers, and their eyes. This is because of the great quantities of red cells in the dissemination.
As the blood is thicker than typical it can’t stream as effectively, particularly through the more modest veins. Whenever left untreated, this expands the danger of the development of blood coagulation inside a vein. Blood clumps are a typical complexity of PV and happen in around 30% of individuals, even before they are analyzed. Draining and simple swelling can likewise happen. This is normally minor and happens in around one-fourth, everything being equal. Types of blood cancer
Essential thrombocythemia
Like polycythaemia vera many individuals have no indications when they are first determined to have ET. Apoplexy (blood clump) is a significant difficulty of ET. Blood clumps can happen in enormous or little corridors, meddling with the blood and oxygen supply to different organs or tissues. More established patients and those with a high platelet count, or an earlier history of apoplexy, might be in expanded danger.
A significant point of treatment in ET is to diminish your platelet count, and subsequently your danger of apoplexy. Less normally, individuals experience manifestations of strange draining including swelling for reasons unknown or misrepresented or delayed draining after minor cuts or injury. In pregnancy, uncontrolled ET can diminish the blood supply to the placenta or baby. This can create issues with fetal development and may now and again prompt an unnatural birth cycle. A developed spleen is normal and happens in around 30% of instances of ET. At times the liver may likewise be augmented (hepatomegaly).
Myelofibrosis
Essentially all patients with myelofibrosis have an amplified spleen (splenomegaly) when they are first analyzed, in spite of the fact that around 20% of individuals will have no manifestations. In around 33% of cases,, the spleen is extremely augmented. Stomach distress can likewise result from an augmented liver (hepatomegaly), which happens in around 66% of cases. Other more uncommon indications incorporate bone and joint torment, and draining issues.
More information about myeloproliferative neoplasms
- MPN diagnosis
- MPN treatment and side effects